Natural Family Planning and Catholic Hospitals: A National Survey
A recent survey conducted by the American Academy of Natural Family Planning (AANFP) found that over 55% of Catholic hospitals surveyed either provide or would like to provide some form of Natural Family Planning (NFP) services. In addition, over 60% of the respondents felt that NFP should be part of the mission of a Catholic hospital. This recent survey was conducted by the AANFP in order to determine the use ofNFP in Catholic hospitals, (i.e., whether NFP is provided, types of NFP methods taught, teaching standardization and methodologies used, qualifications of NFP teachers, and the ethics of NFP services). This article is a report on that survey.
Methodology
A random sample of 349 Catholic hospitals in the United States, (or about 59% of the 590 Catholic hospitals listed in the Catholic Hospital Association 1990 Guidebook) were selected by computer from the membership of the Catholic Health Association. In August of 1991, the Chief Executive Officers (CEO) from each of the 349 hospitals were mailed a NFP questionnaire and a letter explaining the purpose of the survey. The NFP questionnaire was developed by members of the Science and Research Committee of the AANFP. The questionnaire contained a front page of key terms and definitions to facilitate a common understanding of the 34 items included in the survey. After a two week period, the same 349 CEO's were sent a reminder letter and another questionnaire.
Of the 349 hospitals surveyed, 218 or 62.5% responded. The average size of the responding hospitals was 281 beds with 18 bassinets. The hospitals ranged in size from less than thirty beds to over 1,000 and were comprised of all types of facilities including rehabilitation and psychiatric. The positions of the individuals who completed the questionnaire from the 218 hospitals were 73 (33.5%) Administrators (CEO, President, Vice President), 54 (24.8%) Nurse Managers, 22 (10.1 %) Hospital Educators, 22 (10.1 %) NFP directors or practitioners, and 10 (4.6%) were Religious/Pastoral Care personnel. Thirty-seven or 16.9% did not list their positions. Over half of the respondents were registered nurses by profession.
Results
When asked the question, "Do you offer NFP services at your hospital?" 85 (39.0%) responded "yes" and 133 (61.0%) responded "no". Of the hospitals that responded "no", 37 stated that they would like to offer NFP services. This means that over 55.9% of the Catholic hospitals surveyed either provide or would like to provide NFP services.
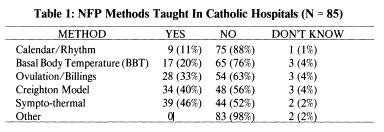
When asked what type of NFP methods are taught in your hospital, the Sympto-Thermal Method was the most frequent response 39 (46%), followed by the Creighton Model (CrM) 34 (40%), and then the Billings Ovulation Method 28 (33%). Since the Creighton Model is a variation of the Ovulation Method, the most frequent NFP method taught in the responding Catholic hospitals is the Ovulation Method. Some hospitals still provide the out-of-date temperature and calendar / rhythm methods. (See Table 1).
NFP Standards
There was a series of seven questions on the NFP questionnaire that addressed use of standardized methodology and practice in providing quality NFP services. A standard is an authoritative statement or set of statements by which the quality of practice can be judged. A majority of the hospital NFP programs state they use established standards N = 74 (87%) and uniform teaching methods and content N = 75 (88%). When asked from what organization these standards have been established 16 (21.6%) responded from Creighton University Natural Planning Education and Research Center, 13 (17.6%) gave no response, 13 (17.6%) stated from the AANFP, 11 (14.9%) from regional NFP programs, 7 (9.5%) from the Couple to Couple League (CCL), 6 (8.1 %) from the Diocesan Development Program for NFP, and 8 were varied responses, including diocese/archdiocese and the World Organization of the Ovulation Method Billings (WOOMB.)
A majority of the NFP programs used both group format N = 53 (63%) and/ or individual format N = 60 (71 %) in teaching NFP. Sixty three of the hospitals (74%) provided special instruction according to the woman's reproductive category in their teaching sessions and 48 (56%) conducted pregnancy evaluations on all of their pregnancy occurrences. Fifty-eight (68%) indicated that an effectiveness study had been conducted on the method that they utilized to teach NFP.
NFP Teachers
The next part of the survey had a series of questions that addressed the characteristics of NFP teachers that the hospitals utilized. Seventy-one (84%) of the hospitals who provide NFP services indicated that they had on-site teachers to provide NFP services. The majority of these NFP teachers N = 50 (70%) are not employed by the hospital, are not salaried N = 53 (74.6%), are not paid through fee for services N = 52 (73%), and do not receive third party reimbursement for services N = 68 (96%). Only 14 (19.7%) of the hospitals had at least one full-time NFP employed teacher. One hospital had three full-time teachers. However, 36 or (50.7%) of the hospitals had one or more part-time employed NFP staff members. Most of the teachers do not volunteer their services N = 47 (66%).
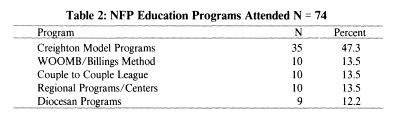
The majority of the NFP teachers in the Catholic hospitals surveyed are certified by an accrediting body N = 64 (75%). Nineteen (29.6%) are certified through the AANFP, 10 (15.6%) through the CCL, 9 (14.1 %) through regional programs, 9 (l4.l %) through Diocesan programs, 5 (7.8%) through Creighton University, 5 (7.8%) through WOOMB, one program (1.6%) stated that they certify their own teachers and six programs (9.4%) did not list the certifying organization. Table Two gives a break-down of the education programs that the NFP teachers attended to learn to provide NFP services. The most frequent programs the NFP teachers attended were the Creighton Model Education Programs (N = 35). Twenty-seven of the 35 attended the Pope Paul VI Institute for the Study of Human Reproduction Creighton Model Education program in Omaha, Nebraska.
NFP and Ethics
The last section of the questionnaire included questions on ethical codes and on issues and opinions related to NFP. Seventy-seven or (91 %) of the hospital NFP programs stated they followed a Code of Ethics. When asked from what source or organization the Code of Ethics came from 19 (24.7%) gave no response, 16 (20.8%) said the AANFP, 10 (13.0%) from individual diocese, 8 (10.4%) said the Catholic Church, 8 (10.4%) said the CCL, 7 (9.l%) said the Hospital Code of Ethics, and 3 (3.9%) said the DDP-NFP. None of the NFP programs provided contraceptive services, only 6 (7%) referred for contraceptive services and one referred for abortion services.
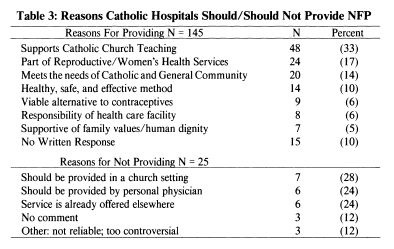
When all 218 respondents were asked "Should Catholic health care facilities provide NFP Services?", 145 (66.5%) said "yes", 25 (11.5%) said "no", 30 (13.8%) responded "don't know" and 18 (8.3%) gave no response. Table 3 gives a break down of the general reasons for the "yes" and "no" responses.
A final question was whether NFP services were a viable alternative to contraceptive services in a Catholic hospital. The majority of the 218 respondents said "yes" N = 137 (62.8%), 25 (11.5%) said "no", 36 (16.5%) indicated "Don't Know", and 20 (9.2%) gave no response.
Discussion
The survey indicated that a majority of Catholic hospitals either provide or would like to provide NFP services. A substantial majority of the respondents also believe that NFP should be offered by Catholic hospitals. The Catholic hospitals that do provide NFP services generally offer the modern methods of NFP, i.e., some variation of the Sympto-Thermal or Ovulation Method. Only a small percentage provide less effective older NFP methods. The fact that 39% of Catholic hospitals provide NFP services and that another 16.9% would like to offer NFP services is an indication that Catholic hospitals are taking the responsibility of providing family planning services that coincide with church teaching and that meet the needs of Catholics and others that prefer natural means to avoid or achieve pregnancy.
One indication of quality of a NFP program is whether the NFP services provided follow recognized standards of teaching. For example, conducting pregnancy evaluations is a standard of practice recognized by both the DDP and the AANFP. The majority of the hospitals indicated that they do follow established standards and utilize uniform teaching content and methods. Over 55% of the hospitals indicated that they conducted pregnancy evaluations.
Another example of providing quality NFP is giving instruction according to the woman's reproductive category. NFP instructions can vary considerably whether the woman is post-partum, totally breast-feeding, weaning, infertile, engaged, coming off of oral contraceptives, premenopausal and so forth. Seventy-four percent of the hospital NFP programs do provide instructions according to the woman's reproductive category.
According to standards developed by the AANFP, an important component of NFP services is whether the program and teachers follow a Code of Ethics. Most of the NFP teachers in Catholic hospitals stated they follow a Code of Ethics and do not provide contraceptive services or refer for contraceptive and abortion services. However, many of the organizations listed as sources for a code of ethics do not have a code for teaching NFP. A Code specific to NFP is important because of the unique nature of providing value based NFP. For example, discouraging the use of barriers (e.g., condoms) during fertile times is a code of behavior for teaching NFP advocated by a number ofNFP organizations.
Whether the NFP code of ethics follow Catholic Church teaching is also important to most of the respondents of the survey. Over 66% ofthe respondents felt that NFP should be provided by Catholic hospitals because NFP reflects Catholic teaching, Catholic sexual ethics and supports the values and mission of the Catholic hospitals. Respondents also felt that NFP was a valuable community service, was supportive of the family and was an essential part of woman's health and reproductive and adolescent services. These views reflect the views of hospital administrators 1,2 and the description of services provided by exemplary NFP programs in the literature.3,4
In summary, a substantial number of Catholic hospitals in the United States provide or want to provide NFP services. The NFP services in many of the hospitals do meet standards of service and the teachers are properly prepared. Seventy-five percent of the hospitals that provide NFP services do so through certified teachers. The NFP programs follow Catholic sexual teaching but many do not have a code of ethics specific to NFP.
In 1981, Daly, Prebil, and Hilgers, said that in the 1980's more and more NFP programs will be developing and that Catholic hospitals are in an excellent position to lead the way.4 They also stated that NFP program development will require a long term approach and not an expectation of instantaneous success. As is evident in this survey, many Catholic hospitals have or wish to have NFP programs. It is also evident that these programs need to continue to grow in providing quality service and qualified NFP teachers. Unlike the early 1980's, hospital programs do not have to start from the beginning and can receive direction from successful. exemplar programs and from professional NFP organizations such as AANFP.
References
- 1. P.F. Cook, Sre. C. Durr, and J.T. Farrel, "NFP in the Health Care Institution," International Review of Natural Family Planning. Fall, 1986.
- 2. Sr. L. Gallahue, "Societal Trends, Church Beliefs Support NFP Methods," Hospital Progress. December 1983.
- 3. "NFP Center Reaches Couples, Teens, Physicians, Parents," Hospital Progress. April 1983.
- 4. K.D. Daly, A.M. Prebil, and T.W. Hilgers, "NFP Programs Provide Consumer Choice, Benefit Hospital," Hospital Progress. October, 1980.
Article copyrights are held solely by author.
[ Japan-Lifeissues.net ] [ OMI Japan/Korea ]