Louise
Note from Ron Panzer: Olivia tells us how her mother, Louise, was hastened to death in a hospice facility. Olivia is a pseudonym used to protect the victim's daughter who is still grieving for her mother who died in 2007 from an intended death involving callous, knowing neglect and the administration of medications which were not needed as well as the deprivation of medications which were needed. This is one more form of stealth euthanasia.
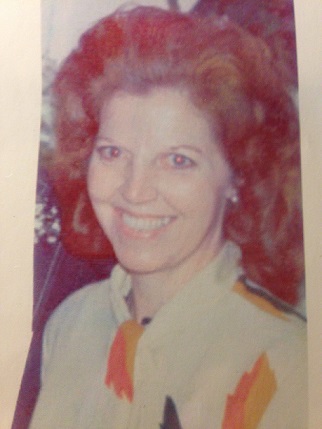
Mom became a widow with three children to raise alone at 30 years old when our father died suddenly. After his death, she worked two shifts most every day to support her young family. My Mom Louise She loved the Lord, and her Bibles were worn. She loved family and friends. Everyone loved her, too. She was kind, patient, loving, generous, smart, a worker bee, and she always made time for her family.
Let me start by saying that I believe hospice care probably can be a helpful service in many instances. I worked in three different hospice agencies officially as a community educator, account liaison, and business development director. I almost always sat-in on all hospice interdisciplinary team meetings for eleven years in these hospices - for-profit and not-for-profit - and in all those years, I never witnessed a medical director or any doctor make a house call and actually examine a hospice patient.
There always was a "revolving door" of newly-hired nurses and nurses leaving who had varying skill levels, abilities, and even vices who served as the intermediary between the medical director and the patient. The doctor relied solely on the nurses' reports and this is common in most hospices today!
At the time of my mom's death, all decisions were made by third-string nurses who were filling in for "second-string" holiday weekend nurses. In hospice, it is known that Christmas is the most deadly holiday for inpatient care. That's actually true for any niche of healthcare. Most temporary holiday staff employees came from outside the community, they had little or no hospice care experience, and they certainly were not familiar with their new patients and their plans-of-care or histories.
In my mother's case, I believe hospice and other healthcare staff almost killed her through intentional neglect the first time she was seen by hospice staff, and the second time hospice was involved, I believe neglect directly resulted in her death. She had a Do Not Resuscitate order ("DNR") and once a DNR is signed, there is very little recourse.
My mom lived alone in Northwest Georgia and various family members would occasionally stay overnight with her due to her declining health caused by chronic obstructive pulmonary disease ("COPD"). Mom was a retired nurse, never smoked a day in her life, had always been in excellent health, and had maintained an ideal weight due to healthy eating habits and exercise.
At the urging of a registered nurse with a local home health care agency, mom signed herself up with their company hospice. It appeared to be a good idea at first, as she was told that her medical expenses would be covered, and she would receive frequent home visits from their hospice interdisciplinary team.
The hospice case manager told mom about their "respite care benefit," so mom agreed to a short-term respite. Respite care is designed to give family members a break, but we were surprised at the arrangement since no one was exhausted nor did we need a break. I believe she thought it would be a nice change of scenery or a short social outing. Mom talked with me on Friday afternoon from her room by cell phone about how much fun she would have visiting other patients while there, and she had hoped to go for a walk before returning home.
Respite care is usually 7 days or less. Unknown to her, or to us, their hospice in-patient contract was with a poorly run inpatient health care facility (nursing home #1) approximately 30 miles east of mom's home and located in a different county. My first reaction was disbelief, because I had heard of the facility's very poor reputation.
While under hospice care, there were two near-death incidents within three months: The first almost ended my mother's life, and the second did end her life!
My observations and experiences:
The first near death incident occurred on Saturday, September 15th, 2007 at the long-term inpatient health care facility with the first hospice contracted to provide care where mom believed she was going to "enjoy" respite care.
On Saturday, September 15, 2007 my daughter and family from Alabama were visiting with me in North Georgia, and we decided to visit mom. My daughter had planned to visit mom while in Georgia, and she was surprised to learn that mom was in respite care. If it had not been for my daughter's visit, no one would have visited mom on Saturday, as we expected her to return home within a couple of days.
At 4 p.m. on Saturday we signed in at the health care facility - the only nursing home in the county - walked into mom's room, where we found her in the full blown dying process. The room temperature was icy cold, her bed was beside the window and the air conditioner was on high. She was tossing from side to side moaning in pain, unable to breath and drawing her breath from the diaphragm. She did not know us! She was unaware of anyone. We later learned that she was close to death.
We looked for her breathing machine, which is used to administer a steroid treatment and there was no machine! Her oxygen tubing was on the floor! She had been told not to bring her breathing machine from home as "everything would be provided." My mom always administered her own breathing treatment, but there was no machine in sight! While my daughter tried to help mom, I ran to the nurse's station a few doors away where I found three medical employees socializing. Not one rushed to her room! They were aware that she was in distress - as she had been all day! The facility medical director and an attending RN/administrator had noted her condition while making morning rounds!
I demanded that an ambulance be called and after several "keystone-cop type employees" filled her room to "sit her up in the bed" - as though this would do any good - the EMT's arrived. Mom was taken across the street to the county hospital ER where she received care. The ER doctor told me that a decision had to be made regarding life support. Although she had signed a DNR, I did not believe that her condition was based on natural causes but rather on neglect.
With my instruction, she received life support in ER, and Mom remained in a coma for two days. Later when I told mom about her near death experience, she was shocked and agreed that life support was indeed needed. That same night, Saturday, when my daughter and niece had a chance to return to the nursing home to retrieve mom's things, they were able to meet and talk with her roommate, who told them that mom's condition had become very serious over Friday night. I firmly believe that the staff did not administer her necessary breathing treatments, that the staff fully knew that she was in distress, and that the staff made a decision to withhold care and "let her die."
I saw for myself that a nebulizer machine and mom's medications were not there which would have allowed her to administer her own treatment. Mom's roommate was so worried about her, and she had tried to get help from the staff. Frustrated, mom's roommate sought prayer for her during a Saturday afternoon worship service.
Why Weren't We Called?
If mom had died, we would have been clueless as to cause of death. How often does this happen? From my experience and seeing how the staff acted, I believe it happens frequently!
The nursing home medical director, also had hospital privileges, and he refused to release or transfer mom to another hospital. We were afraid to leave her for even one minute after this nightmare. My brothers, sister and I had mom transferred by ambulance, against the same doctor's orders, to our hometown ER where she was examined and released to go home. The out of town ambulance staff EMTs who transferred mom were not surprised by our story, and they were fully aware of this doctor's reputation.
Because mom was discharged from the first hospice due to her hospitalization, she did not return to their care, and we didn't want her to return there.
A few days later - and much weaker due to her near death experience - we agreed to a referral from our local hospital's case manager, and mom signed up with the second hospice located approximately 30 miles South in another county. Mom stayed at home where she thrived until the second hospice intervened again.
The last night I spent with my mom was Monday, December 17, 2007. She was feeling very excited about Christmas, and she was up and about wrapping presents for her grandchildren on Tuesday the 18th. I left for Alabama with plans to return on Saturday morning, December 22nd. On Thursday evening I received a call from my mom indicating that the nurse from the second hospice had been by and suggested that she check into their inpatient facility. This surprised everyone, but we were not overly concerned as this had happened before for symptom control and seemed routine.
This hospice had opened an in-patient unit where the physical conditions were much better - or at least we believed the conditions to be better. Mom expected to return home no later than Sunday, December 23rd. On Friday, December 21st my brothers spent the day with mom at the hospice facility. She sent them to K-mart to buy hair pins, chocolate and new pajamas. They left in late afternoon and mom was funny and feeling fine. Had there been any sign of trouble, someone would have stayed overnight.
My aunt last talked with mom that same night at 8 p.m. and again she was fine. On Saturday 22nd according to her Certified Nursing Assistant (CNA), and mom's chart, she was resting peacefully at 6 a.m., but at 7:15 a.m., the CNA said she found mom on the floor wrapped around the nightstand. She called for help and the staff assisted the CNA in returning mom to bed. The CNA said that mom kept apologizing for falling and causing any trouble. According to the CNA, Mom was complaining of pain but no one checked her body for injury from the fall. At 8 a.m. my brother called to speak with mom and was told that she was asleep and still no one indicated that she was in trouble.
No member of the hospice staff ever called anyone of us - her own children - about the fall or her condition!
She died around 10 a.m. "peacefully," and I received a call from my sister-in-law while in route home to Georgia for what was to be a fun Christmas with my mother.
When I reviewed mom's chart after her death, I was shocked to see that the staff had never mentioned anything about the fall, her pain, or any other problem! When I examined her body before it was removed, I noticed that the top of her left hand was black and her left little finger appeared broken. I have a photo which was taken before the coffin was closed…it reveals the finger and bruising. I am certain that these injuries would have caused her to complain of pain. I believe that she was over-medicated and with the sedatives given to in-patients to help them sleep, she probably got up to do a breathing treatment. She must have struggled to find her machine and medications and she may have fallen due to her over-medicated state. No middle of the night breathing treatment was recorded in her chart. I returned unannounced to review mom's chart first thing following her death early Sunday morning.
Normally she would require a 20 minute treatment every 4 hours. But if heavily drugged, she would not have been able to stay awake to hold her own treatment even if she had been provided such a treatment. I believe that if she had received a breathing treatment she would not have died. I do believe that she was over-medicated and opioid pain meds along with Ambien sedative, and other medications stopped her breathing and her heart! I had spent many nights with mom in her room, and I knew the drill. After she took a breathing treatment, she would always return to a sound sleep.
It is a mystery as to why she needed to return to in-patient care. I speculate it was because the hospice field team would be short staffed during the weekend and holidays. She died on a Saturday before Christmas, and the odds were against her! From my work experience in health care facilities, I have observed that death rates soar on weekends and holidays due to part-time help!
I filed a report with the State ombudsman shortly after the first incident. Sadly nothing came of it. Many government programs accomplish nothing and fail to protect anyone!
March 1, 2009 Entry - There was a dark circle of bruising around my mom's neck when she died. I brought up the bruising for discussion with my aunt, and she told me…that she had adjusted mom's head forward from a backward tilted position after her death and the movement could have caused the bruising. This seemed acceptable to me at the time - until recently. While watching TV, I heard a pathologist explain why the body does not bruise after death! Now I have more questions than answers about mom's final hours.
One more thing … While in the 2nd hospice's in-patient unit some time before her final admission, she shared something that had occurred, and until now it didn't seem to be all that important. She told me one night she was awakened by a man who worked at hospice. I don't know if he was a CNA or maintenance man? She said he had a small flashlight and was standing beside her bed in the dark.
When she spoke to him, he said he was looking for something. Although she was always given a sleeping pill (Ambien) at night, she was certain about her experience with the man in the room, and it made her uncomfortable. Note - Mom's mind was sharp, she NEVER experienced dementia, and was fully aware of everything.
Note from Ron Panzer:
Any time a patient's life is ended through negligence, abuse, or consciously imposed death, but the death is not recorded as a crime or "euthanasia," that medical killing is an example of stealth euthanasia which is pervasive in a health "care" system that is increasingly becoming hostile to life. These are the signs of the culture of death. If you wish to understand how hospice was intentionally tainted, see the Four Part Wesley J Smith, JD/Ira Byock, MD Expose'.
Patients, family members, and patient advocates need to recognize the signs that should be "red flags" warning them that the staff are not listening to the patient and respecting their wishes. Hopefully, that is not the case, but if it is, we must remember that the patient always has the right to refuse an unwanted and unneeded medication or treatment. The right to refuse is a power that still resides within the patient, closest family member, or patient advocate who has the medical power of attorney. If we stand firm and assert this right under law, the staff cannot legally administer those unwanted medications or treatments. If they still insist, then that is an indication it is time to look for another agency or faciiity that will honor the patient's wishes.
In some cases, if a pro-life hospice can be found (they are becoming rarer and rarer), that would be the best solution for a patient clearly suffering from an end-stage disease recognized as bringing the patient near to the end-of-life. If one cannot be found, consider a home healthcare agency. Many famiies and patients are lured into hospice with the promise that the hospice will "provide everything for free," but what good are free services when the patient is already dead due to an imposed death that is hastened by the staff? Listen to your instincts, your intuition, what all logic tells you is happening, and if it does not appear to be right, then it's time to terminate the services of that hospice or other agency.
If you decide to terminate services, do not tell the hospice staff you intend to terminate services until you have found another agency and let them tell the hospice staff! Never raise your voice or act angrily to them. Some family members have actually been "banned" from seeing their own loved ones, because the hospice did not wish to cooperate! Simply state the patient's wishes about medications or treatments calmly but firmly without wavering.
Look for another agency and have them arrive on site with admission papers already drawn up to transfer care into their service. Let them explain that they have already taken over and have assumed care (and will transport the patient right then if this is in a faciiity). If the patient will be going into home health care, the hospice benefit is "revoked" at that time (not before the other agency is already on site and ready to take over), and the patient goes back to regular Medicare (if on Medicare).
Once a patient is "in the system," a patient requiring care cannot simply "go home" without an agency supervising or following the patient and making sure the care and medical orders are being implemented. That would be considered "abandonment" in the eyes of the authorities (like social services and health care department). This is why one needs to arrange for another agency to take over. Home health care agencies are much less likely to hasten death. Make sure whatever agency you go to is not affiliated with the agency or health care or regional system you are using that is ignoring the patient's wishes!
Article copyrights are held solely by author.
[ Japan-Lifeissues.net ] [ OMI Japan/Korea ]